Psoriasis is a chronic autoimmune condition that affects nearly 8 million people in the United States. Do you or someone you know struggle with psoriasis? If so, Florida Dermatology and Skin Cancer Centers would like to share important information regarding psoriasis, including causes and factors, treatment options, and tips for daily management. Keep reading to learn more.
What is Psoriasis?
Psoriasis is an inflammatory skin condition without a known cure. However, psoriasis is treatable and manageable with a combination of prescribed medications, lifestyle changes, and alternative therapies and regimens.
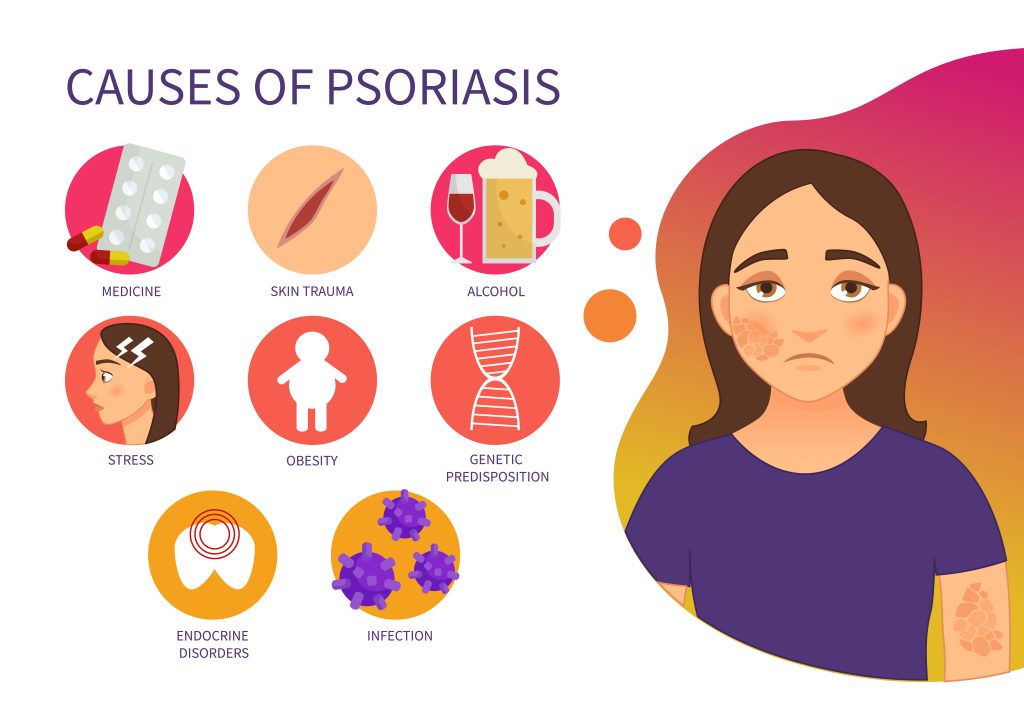
Psoriasis is thought to be caused by an immune system disorder that triggers inflammation and increased skin cell growth and turnover. When you have psoriasis, your body’s white blood cells (T cells) actually attack your skin cells by mistake. The result? Thick, scaly patches develop on the skin’s surface. Researchers aren’t entirely sure what causes this overreaction of the immune system, although most believe a combination of genetic and environmental factors play a role. For example, if someone in your family has or had psoriasis, you may be more likely or have an increased risk of developing it too.
Psoriasis can affect men, women, and children of all ages, and sometimes runs in families. Psoriasis flare-ups typically come and go in cycles that last weeks, months, or years. Environmental triggers like infections, skin injuries (cuts and scrapes), stress, weather changes, or certain medications can cause a new flare-up.
Types of Psoriasis & Associated Symptoms
There are several different types of psoriasis, including: plaque psoriasis, nail psoriasis, guttate psoriasis, inverse psoriasis, pustular psoriasis, and erythrodermic psoriasis.
According to the American Academy of Dermatology (ADA), plaque psoriasis is the most common type of psoriasis. Common signs and symptoms can vary from person to person and may include red and inflamed patches of skin with thick, silvery scales, skin plaques that itch, burn, crack, or bleed; and dry, thick, pitted fingernails. Plaque psoriasis frequently occurs on areas such as joints, but can also develop on the palms, soles of feet, face, scalp, elbows, and knees. For other types of psoriasis, such as inverse psoriasis, you may notice patches under armpits or breasts, in your groin, or around certain skinfolds.
A flare-up of any type of psoriasis can range in size from small areas with plaque development, to a major outbreak that cover large areas of skin.
Psoriasis is not contagious. It is typically associated with multiple health complications, including psoriatic arthritis and other chronic conditions like obesity, diabetes, heart disease, high blood pressure, and high cholesterol.
How is Psoriasis Diagnosed?
Psoriasis should be properly diagnosed by a licensed medical professional during a dermatologic exam. If psoriasis is suspected, a doctor can take a biopsy, which is a small sample of the affected skin, and send it in for an analysis at a laboratory.
How is Psoriasis Treated?
Multiple treatment options are available to help slow skin cell growth, remove plaques, reduce signs and symptoms, and ease discomfort. Common treatment methods include:
- Topical creams and ointments including corticosteroids
- Biologic medication injections
- Oral retinoids
- Immune-suppressing medications
- Light therapy
Tips for Managing Psoriasis and Controlling Flare-Ups
If you’re living with psoriasis, there are several things you can do at home to prevent flare-ups and manage symptoms.
- Bathe and moisturize daily. Bathe daily using lukewarm water and gentle, fragrance-free soaps and body washes. After bathing, apply a gentle moisturizer to keep your skin from dying out and itching.
- Seek sunlight. Exposure to sunlight can help improve psoriasis, but only a controlled amount. Work with your dermatologist to determine the safest and healthiest way to get sunlight daily. Remember to practice proper sun safety.
- Know your triggers. Know your triggers and avoid them to reduce the risk of flare-ups. Common triggers may include eating red meat, refined sugar, dairy, and processed foods, as well as consuming alcohol, taking certain medications, smoking, or getting a viral or bacterial infection. Having a hormonal imbalance or a skin injury can also trigger an outbreak. You may find it useful to keep a journal documenting triggers and flare-ups to help you navigate common triggers.
- Talk to a professional. Many people with psoriasis develop mental health issues like low self-esteem, depression, and anxiety related to their condition. If your mental health is suffering due to psoriasis, seek counseling from a licensed therapist.
- Manage stress. Stress is the primary trigger for flare-ups. Consider practicing healthy habits and following routines that help you lower your daily stress levels.
Overall, living a healthy lifestyle and reducing stress can help you manage your condition and improve your quality of life.
Next Steps
Sometimes it can be difficult dealing with the symptoms and management of a complex condition such as psoriasis. With this, the team of experts at FLDSCC wants to help you manage your psoriasis to the best of your ability.
For more information about services that Florida Dermatology and Skin Cancer Centers provides, or to make an appointment for a skin exam, visit www.fldscc.com or contact us at (855) FLD-SKIN.


