When it comes to information surrounding skin cancer, especially melanoma, it can be hard to determine fact from fiction. Luckily, many organizations like the American Academy of Dermatology and the Skin Cancer Foundation regularly disseminate helpful learning materials to debunk myths and uncover truths about sun exposure and protection, as well as skin cancer awareness.
Learning more about how to protect yourself from skin cancer and knowing what to look for when it comes to the health and well-being of your skin can make a world of difference. Following a simple, yet effective skin and sun care routine can help limit your chances of developing skin cancer and help keep you looking and feeling your best.
We recognize that even if you are equipped with all the right information, common questions may still arise that could leave you feeling puzzled. To aid you in making the best decisions for your skin, we are going to break down the below and debunk the myths surrounding sun safety and melanoma.
Melanoma FAQ’s
Q: What causes melanoma?
A: Melanoma is primarily caused by overexposure to UV radiation from the sun or tanning beds, which damages the DNA in skin cells. While sunburns and UV exposure are significant risk factors, melanoma can develop in people who have never had a sunburn. Genetics, a weakened immune system, or the presence of unusual moles can also contribute to melanoma risk, regardless of sun exposure. This myth can lead to a false sense of security, so it’s essential to stay vigilant about skin health even if you rarely burn.
Q: What does melanoma look like?
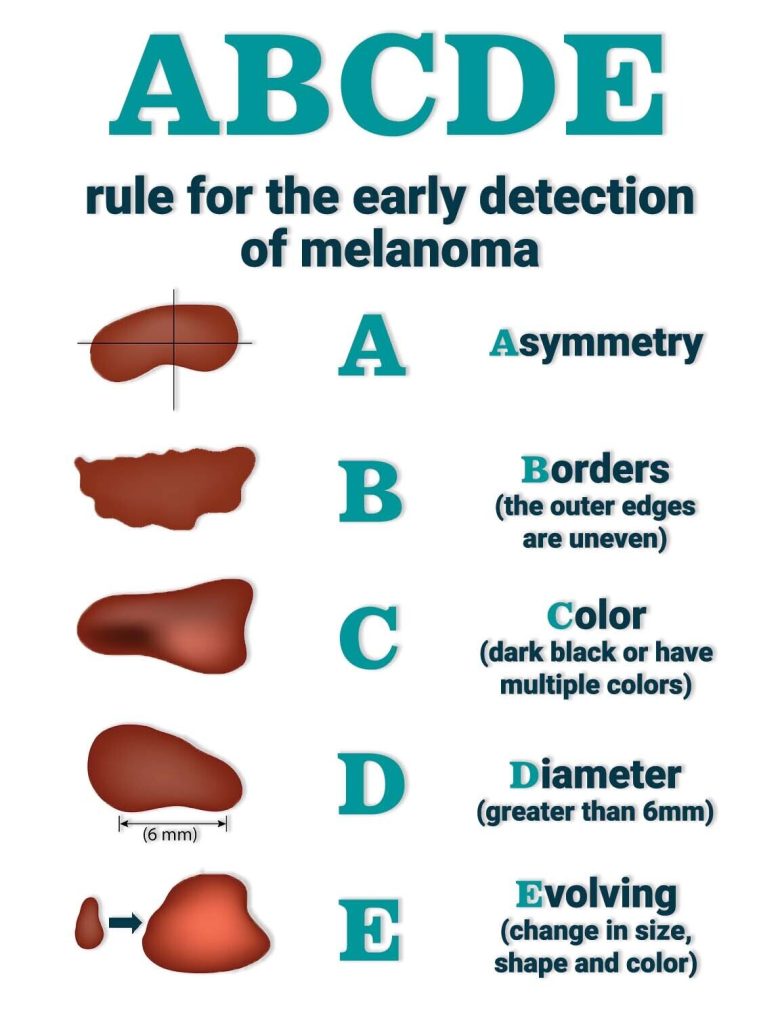
A: Melanoma can appear as a new or changing mole or dark spot, often irregular in shape, with uneven color, or an asymmetrical border. It may look black, brown, pink, or even red and can sometimes bleed, itch, or become tender. The “ABCDE” rule can help: look for asymmetry, irregular borders, multiple colors, diameter larger than a pencil eraser, and any evolution in size, shape, or symptoms. A dermatologist can assess spots that show these signs.
Q: Is melanoma genetically inherited?
A: According to the American Cancer Society, your risk of melanoma will be higher if one or more of your first-degree relatives has had melanoma. About 10% of all people with melanoma have a family history of the disease. If you have a family history of melanoma, it’s imperative that you receive an annual skin exam with a trusted dermatology expert to check for any alarming changes.
Q: Does skin cancer only come from sun exposure?
A: It’s true that sun exposure makes up the majority of melanoma cases. However, other risk factors include genetics, age, and immune health. As mentioned above, you can be genetically predisposed to having melanoma even if you are careful in the sun. Additionally, if you have already had melanoma, your likelihood of reoccurrence will increase significantly.
Q: Can you become addicted to the sun?
A: According to multiple research studies, the more time you spend in the sun, the more beta-endorphins are produced. These endorphins travel through your blood into your brain and stimulate serotonin levels that create “reward pathways” and feelings of euphoria. Addiction to the sun can be a real thing for some people. The problem is that prolonged exposure to UV rays is extremely harmful and increases your risk of developing types of skin cancer such as melanoma. If you find yourself becoming addicted to the sun, you can try other endorphin-releasing activities such as exercise or meditation.
Q: Does sunscreen fully protect me from skin cancer when I am exposed to the sun?
A: The majority of skin cancers are caused by excessive exposure to UV rays. According to the American Cancer Society, even while wearing a broad-spectrum sunscreen, some UV rays can still get through the “filter” of an SPF. Because of this, sunscreen is only considered one part of following a smart sun safety plan. Other habits you should adopt are staying in the shade, covering up with long-sleeved clothing, and wearing a hat and sunglasses. If you can, try to avoid the sun altogether between 10 a.m. and 4 p.m. when the sun is at its highest intensity. Be sure to choose sunscreen with an SPF of 30 or higher, and reapply every two hours, or directly after swimming or sweating.
Q: Does melanoma only affect those with lighter skin?
A: Because of the presence of a lower level of melanin (brown pigment) in those with a lighter complexion, people with fair skin are at higher risk for sunburn, sun damage, and skin cancer. However, UV exposure to any skin type or ethnic group can cause melanoma, including darker-skinned individuals. Just because you don’t get a sunburn or see visible signs of sun damage on your skin, doesn’t mean you aren’t still at risk of developing skin cancer.
Q: Don’t I need sun exposure to get enough vitamin D?
A: While it’s true that vitamin D is a naturally occurring nutrient that comes from the sun, it’s not wise to try to get your daily dose from prolonged time spent under UV rays. A much safer way to ensure your vitamin D is at an optimal level is to speak with your primary care physician about getting a blood test. If you need more vitamin D, you and your physician can work hand-in-hand on a plan that includes taking supplements, eating certain foods, and exercising regularly.
Q: Does my immune system make me more susceptible to developing melanoma?
A: Having a weakened immune system can increase your susceptibility to melanoma. The immune system plays a critical role in identifying and eliminating abnormal cells, including potentially cancerous ones. When the immune system is compromised due to conditions like HIV, certain autoimmune diseases, or immunosuppressive medications, the body may struggle to control the growth of abnormal cells, making it easier for cancers, including melanoma, to develop. For individuals with weakened immune systems, regular skin checks and vigilant sun protection are especially important for early detection and prevention.
It is our hope that with the above information, you will be better equipped to create and follow a sensible care plan before heading outdoors.
Florida Dermatology and Skin Cancer Centers provides a full spectrum of dermatology and skin care services, and its team of physicians, ARNPs, and PAs are experts in diagnosing and treating skin cancers with the latest technological options. Dr. K. Wade Foster is fellowship-trained in Mohs surgery, the most effective technique for most types of skin cancers, with minimal scarring or risk.
FLDSCC brings an unmatched level of services to all our patients, and we are confident in our approach to treat skin cancer most effectively and efficiently. Fortunately, skin cancer treatment, specifically melanoma, has a very favorable outcome since if it is detected early, it’s almost always treatable.
For more information about services that Florida Dermatology and Skin Cancer Centers provides, or to make an appointment for a skin exam, visit www.fldscc.com or contact us at 863.293.2147.


